Diabetic Retinopathy results from damage to the small blood vessels in the retina and is the most frequent cause of new blindness among adults aged 20-74 years old. However, with early diagnosis and treatment, progression of the disease and its associated vision loss can be slowed, and in many cases can be prevented. Diabetic Retinopathy tends to appear and progress in stages beginning with Mild Nonproliferative Retinopathy, progressing to Moderate Nonproliferative Retinopathy, further advancing to Severe Nonproliferative Retinopathy and without proper attention progressing into the most severe stage, Proliferative Retinopathy.
Mild Nonproliferative Retinopathy- This is the earliest stage and is characterized by the presence of “dot” and “blot” hemorrhages and “microaneurysms” in the retina which can be present without any change in your vision and typically does not require treatment unless it progresses or is accompanied by Diabetic Macular Edema.
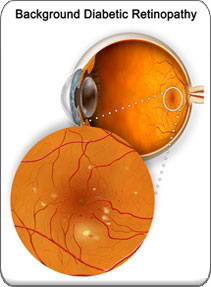
Moderate Nonproliferative Retinopathy-This is the second and slightly more severe stage with more extensive changes whereby some of the small blood vessels in the retina may become damaged enough so that they close off and diminish nutrients and oxygen to certain areas of the retina that is called ischemia.
Severe Nonproliferative Retinopathy-This next stage is characterized by an extensive amount of retinal blood vessel damage and ischemia with patients at a high risk of going to the next stage of retinopathy-the proliferative stage.
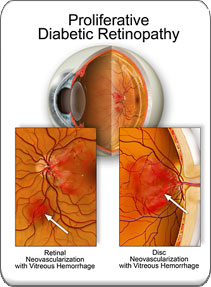
Proliferative Retinopathy-This is the most severe stage and has a significant risk of vision loss. To compensate for the lack of oxygen, areas of the retina send signals to stimulate the growth of new abnormal and fragile blood vessels in order to try and reestablish the supply of oxygen-called neovascularization. These vessels tend to break and hemorrhage into the vitreous gel and can scar and cause retinal detachment, with catastrophic vision loss. It is critical that this stage be treated as quickly as possible in order to stop the progression and preserve good vision.
Diabetic Macular Edema-Leakage from the retinal blood vessels may cause the center of the retina, a condition called Diabetic Macular Edema (DME) which can occur in any stage. It is possible to have Diabetic Macular Edema and not have vision loss.
Routine eye exams including dilated retinal exams and retinal photos should be scheduled for al patients with diabetes on a minimum of an annual basis and more often as suggested by your eye physician depending on the health of the retina. The most effective and accurate ways to observe and diagnose diabetic retinopathy, including Diabetic Macular Edema (DME) are to perform Optical Coherence Tomography (OCT) and Intravenous Fluorescein Angiography (IVF) which we will recommend again as needed to help preserve the health of the retina.
Depending on the stage and the potential for and the degree of vision loss it is possible to treat, stabilize and often reverse the effects of diabetic retinopathy. Treatment of diabetic retinopathy can use retinal laser photocoagulation treatment as well as intravitreal injections of Vascular Endothelial Growth Inhibitor (VEGF) Drugs such as Lucentis® or Eylea®, or a combination of both. Optimal results require early detection ad diagnosis for treatment. Intravitreal injections of VEGF Inhibitor drugs are less destructive than retinal laser treatment and thus are more often recommended as the primary treatment for management of vision threatening complications of diabetic retinopathy.