Glaucoma is an eye disease that is most commonly caused by an elevated pressure inside the eye-intraocular pressure (IOP)-that damages the optic nerve and causes loss of vision. Glaucoma can begin without any symptoms or obvious loss of vision and if not diagnosed early, treated properly and controlled, it will result in permanent vision loss and potentially blindness. There are two main types of Glaucoma: Primary Open Angle Glaucoma (POAG), and Angle Closure Glaucoma.
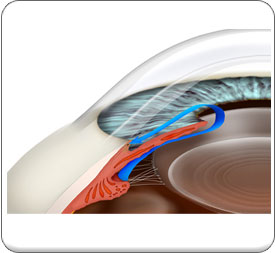
The most common type of glaucoma is Primary Open Angle Glaucoma (POAG) whereby the production and/or drainage of fluid inside the front of the eye-called aqueous humor-is imbalanced, resulting in an elevation in eye pressure (IOP) so that the circulation in the optic nerve becomes compromised, depriving it of oxygen and nutrients causing permanent changes and even damage to the optic nerve, which if left untreated result in vision loss and ultimately blindness.
Primary Angle Closure Glaucoma accounts for about 10% of all cases of glaucoma and about 2/3 of these produce no symptoms for patients.
Acute Angle Closure Glaucoma is one of the only types of glaucoma that produces distinct symptoms that include pain, light sensitivity, redness, blurred vision, colored haloes around lights and nausea or vomiting. Acute Angle Closure Glaucoma is considered a medical emergency. If you experience a sudden onset of pain, redness, blurred vision, light sensitivity, haloes around lights, nausea and vomiting, please call Doctor & Associates at 203-227-4113 and relay these symptoms to the receptionist so that you can be given an appointment immediately. In the event that you are at risk for Angle Closure Glaucoma or in the event that you have Acute Angle Closure Glaucoma we may initially prescribe some medication to begin to lower the pressure but will also perform a type of glaucoma laser procedure called Laser Iridotomy to produce a small opening or hole in the Iris so that Aqueous Humor can drain from the eye more effectively.
Depending on your general health, eye health and family history there are a number of factors that that may influence your likelihood of developing glaucoma. These include the following:
- High Intraocular Pressure
- Age-Risk increases after the age of 40 and is 6x more likely to get glaucoma if you are over 60.
- Race-African-Americans have a six to eight fold increased risk for glaucoma.
- Myopia-Severely nearsighted people have a higher risk of developing glaucoma.
- Hypertension or High Blood Pressure
- Diabetes
- Family History-Any family history of glaucoma is considered a very significant risk factor.
- Early Menopause
- Sleep Apnea
- Thin Corneal Tissue
- Eye Trauma
- Steroids




