There are many conditions that can affect the cornea such as Keratoconus, Fuchs’ Dystrophy and Herpes Keratitis. Most of these eye conditions and corneal diseases can often be treated using non-surgical treatment options. However if they are not diagnosed and treated early or if they progress to where vision is compromised beyond an acceptable level, it may be necessary for Dr. Doctor to perform a Corneal Transplant.
Corneal Infections, Herpes Simplex & Zoster Keratitis
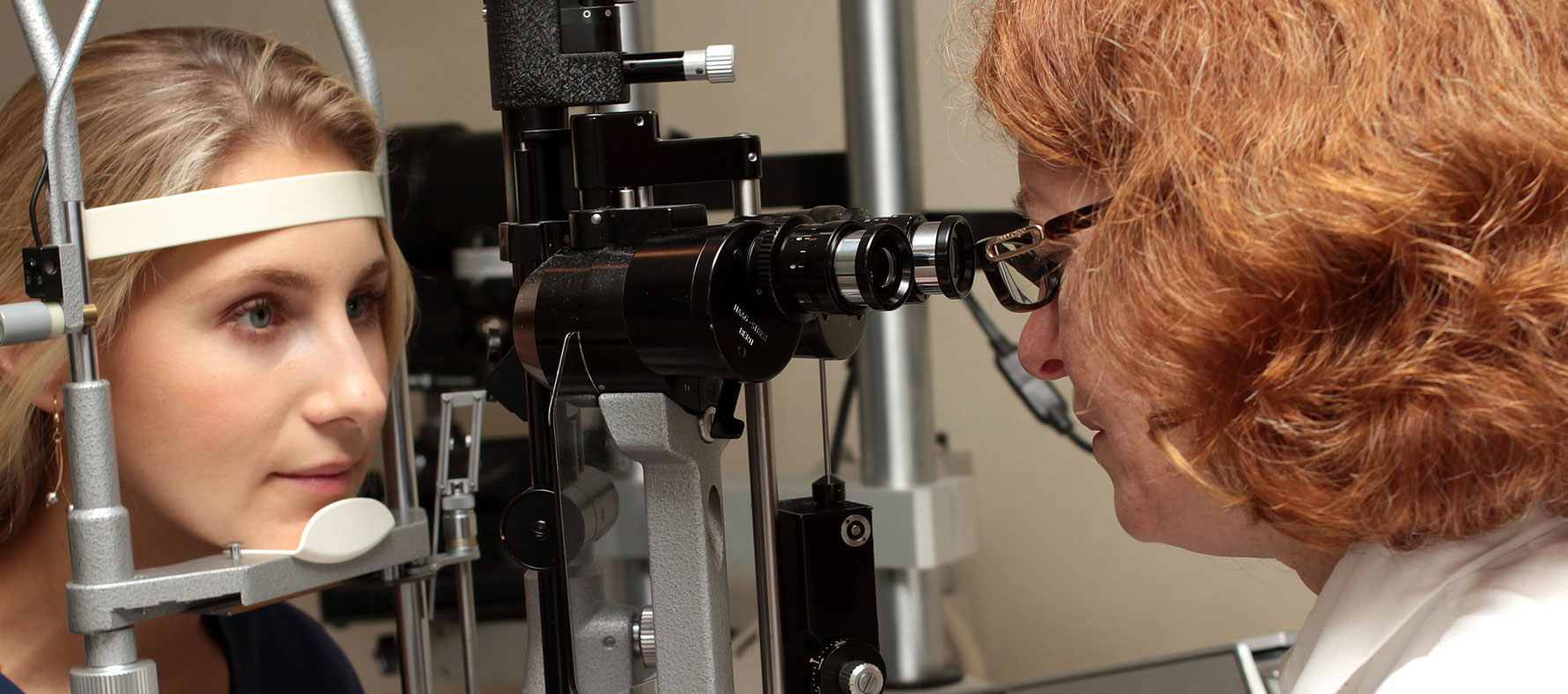
Corneal infections are a potential cause of discomfort and vision loss if not diagnosed and treated promptly. An infection of the cornea is called Keratitis. Keratitis can cause a painful inflammation with a discharge, which if not treated quickly and appropriately, can lead to corneal erosion, corneal ulceration and corneal scarring. If Dr. Leslie Doctor suspects that you have a corneal infection, she will look for certain diagnostic signs to help decide the best course of treatment which might be an antibiotic eye drop, an antifungal eye drop, an antiviral eye drop and sometimes it might even include a steroid eye drop to reduce the inflammation.
Herpes Zoster Keratitis is caused by the same virus that causes chicken pox, called Varicella-Zoster Virus. It is possible that after having chicken pox as a child, the Varicella-Zoster Virus remains in the nerve cells of your body in an inactive state and can reactivate later in life and travel through the nerves in different parts of your body causing a painful blistering rash. If the Varicella-Zoster Virus travels to your head or neck it can affect the eye and thus cause a corneal infection.
Ocular Herpes, or Herpes of the eye is caused by the Herpes Simplex Virus and is the most common causes of corneal blindness in the United States today. Up to 50% of people who have a single Herpes Simplex viral infection of the eye will experience a flare up or recurrence. The virus often leads to irreversible scarring of the cornea. Ocular Herpes may start as a painful sore on the eyelid or surface of the eye. If left untreated, it may multiply and begin to destroy epithelial cells and progress deeper into the cornea. If the Ocular Herpes penetrates the deeper layers of the cornea it may cause corneal scarring-so prompt diagnosis and treatment of Ocular Herpes is important.
Fuchs’ Dystrophy is a slowly progressive disease of the cornea that occurs when the innermost layer of cells, called the endothelium, prematurely weakens, making it less efficient in its “pumping activity” which is required to maintain transparency for clear vision. Sometimes we may observe Fuchs’ Dystrophy in people in their 30’s and 40’s, but most often does not compromise vision until people are in their 50’s or 60’s. Early in the course of Fuchs’ Dystrophy you may wake up with blurry vision that gets progressively clearer as the day passes. In its later phases, Fuchs’ Dystrophy is often associated with considerable pain as the epithelium blisters called “bullae.” Many patients with Fuchs’ Dystrophy that require surgery to restore vision may benefit from a technique called Descemet’s Stripping with Endothelial Keratoplasty (DSEK). This type of corneal transplant involves only the diseased portion of the cornea and is sutureless.
Map-Dot-Fingerprint Dystrophy is a corneal condition affecting the outermost layer of the cornea, called the epithelium. It is attached to an underlying basement membrane called Bowman’s Membrane. Sometimes the epithelial basement membrane develops abnormally making it difficult or impossible for the epithelium to adhere properly to the basement membrane. If the epithelium does not adhere properly, Recurrent Corneal Erosions will occur. Recurrent Corneal Erosions are painful and cause the corneal surface to become irregular resulting in intermittent blurry vision along with the discomfort and foreign body sensation. Map-Dot-Fingerprint Dystrophy is also known as Epithelial Basement Membrane Dystrophy because it is caused by a lack of the healthy formation of the Basement Membrane. It affects adults between the ages of 40-70 and can sometimes begin earlier. As the name implies, its appearance is of a map of gray areas accompanied by opaque dots and fingerprint like whirls or lines. The best treatment results can be achieved using Excimer Laser Phototherapeutic Keratectomy (PTK) to smooth the surface of the cornea.
Lattice Dystrophy occurs from the accumulation of abnormal protein fibers, or amyloid deposits in the middle cornea layer called the corneal stroma. If these deposits become dense enough they will become opaque and affect the corneal transparency so that vision is reduced. If these deposits occur under the outermost layer, the epithelium, they can cause recurrent erosions of the cornea, which can be painful and disturb the normal corneal curvature, effecting vision. In instances where there are recurrent corneal erosions and pain, the doctor may prescribe eye drops, ointments and occasionally an eye patch or bandage soft contact lens. Early Lattice Dystrophy seems to respond well to Excimer Laser Phototherapeutic Keratectomy (PTK) whereas more serious cases may require a corneal transplant.
Pterygium
A pterygium is a fleshy triangular growth of tissue on the cornea that may grow slowly throughout a person’s life. Rarely, a pterygium can grow across the cornea and block the pupil. People who live in sunny climates where they are exposed to more sunlight and UV light are more prone to developing pterygia. Pterygia may become red, swollen and inflamed. Occasionally they need to be removed. Removal of a pterygium is a surgical procedure that has recently undergone medical advances. Dr. Leslie Doctor uses a surgical technique called Amniotic Membrane Graft in order to prevent recurrences and obtain the best possible results for Pterygium surgery.
Corneal Transplants
A corneal transplant is a type of corneal eye surgery performed in order to replace diseased, damaged or scarred corneal tissue with new healthy corneal tissue. Since damaged or scarred corneal tissue does not allow light to effectively pass into the eye and reach the retina, poor vision and even blindness may result from a damaged cornea. There are several types of corneal transplants Dr. Doctor my use to replace unhealthy corneal tissue.